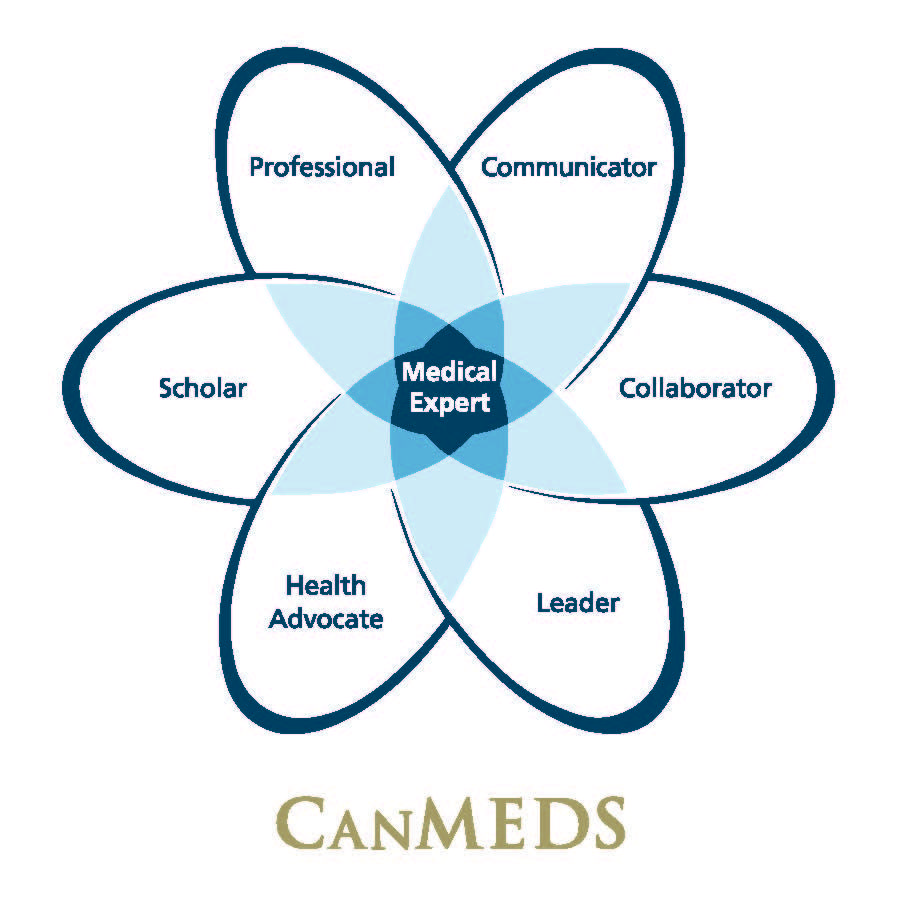
The CanMEDS Framework
CanMEDS is a physician competency framework that identifies and describes the abilities physicians require to effectively meet the health care needs of the people they serve. As the foundation for all Royal College educational standards for specialty education in Canada, the goal of CanMEDS is to improve patient care by enhancing physician training.
CanMEDS – Psychiatry
At the completion of training, the resident will have acquired the following competencies and will function effectively as a:
Medical Expert
Definition:
As Medical Experts, Psychiatrists integrate all of the CanMEDS Roles, applying medical knowledge, clinical skills, and professional attitudes in their provision of patient-centred care across the lifespan and in inpatient, outpatient, and community settings. Medical Expert is the central physician role in the CanMEDS framework.
Key and Enabling Competencies: Psychiatrists are able to…
- Function effectively as consultants, integrating all of the CanMEDS Roles to provide optimal, ethical, and patient-centred medical care
1.1. Perform a consultation, including the presentation of well-documented assessments and recommendations in written and/or oral form in response to a request from another health care professional
1.2. Demonstrate effective use of all CanMEDS competencies relevant to Psychiatry
1.3. Identify and appropriately respond to relevant clinical issues arising in patient care, including:
1.3.1. Awareness of factors influencing the patient’s reactions to the physician and others
1.3.2. Awareness of one’s own reactions when dealing with patients, including the suicidal, depressed, psychotic, demanding, violent, hostile, silent, or withdrawn patient
1.3.3. Boundary issues
1.3.4. Burden of medical, surgical, and psychiatric illness to individuals, families, and systems
1.3.5. Capacity/competence
1.3.6. Confidentiality
1.3.7. Comorbidity: medical, psychiatric, developmental; substance abuse
1.3.8. Consent
1.3.9. Culture and spirituality
1.3.10. End-of-life issues
1.3.11. Family issues
1.3.12. Legal and forensic matters
1.3.13. Long-term illness and rehabilitation
1.3.14. Psychiatric manifestations of medical and neurological illness
1.3.15. Stigma
1.3.16. Suicide, self-harm, or harm directed towards others
1.3.16.1. Assessment and management of safety/risk for patient and provider in all settings
1.3.16.2. Policy, procedure, and practice dealing with patient and provider safety, including violent and potentially violent situations in all settings
1.3.17. Systems issues
1.3.18. Therapeutic alliance
1.3.19. Trauma, abuse, or neglect, including but not limited to intimate partner violence 1.4. Demonstrate the ability to prioritize professional duties when faced with multiple patients and problems
1.5. Demonstrate compassionate and patient-centred care
1.6. Recognize and respond to the ethical dimensions in Psychiatric decision-making
1.7. Demonstrate Psychiatric expertise in situations other than patient care, such as providing expert legal testimony or advising governments, as needed
2. Establish and maintain clinical knowledge, skills, and attitudes appropriate to their practice
2.1. Establish, apply, and maintain knowledge of the clinical, socio-behavioral, and fundamental biomedical sciences relevant to Psychiatry across the lifespan and at the designated level of introductory, working knowledge, or proficient, for purposes of core competence
2.1.1. Psychiatrists will be proficient in the following:
2.1.1.1. Etiology, symptoms, course of illness, and treatment of:
2.1.1.1.1. Anxiety disorders
2.1.1.1.2. Bipolar and related disorders
2.1.1.1.3. Depressive disorders
2.1.1.1.4. Neurocognitive disorders
2.1.1.1.5. Obsessive-compulsive and related disorders
2.1.1.1.6. Personality disorders
2.1.1.1.7. Schizophrenia spectrum and other psychotic disorders
2.1.1.1.8. Substance-related and addictive disorders
2.1.1.1.9. Trauma- and stressor-related disorders, and other conditions that may be the focus of attention (V codes)
2.1.1.2. Health care and other regulations, including but not limited to legislation pertaining to mental health, privacy and confidentiality, child welfare, dependent adults, and young offenders
2.1.1.3. Normal and abnormal development
2.1.1.4. Normal aging
2.1.1.5. Normal and abnormal psychology
2.1.1.6. Nosology
2.1.1.7. Psychopharmacology and somatic therapies
2.1.1.8. Psychotherapeutic constructs: individual, family, and group
2.1.1.9. Referral patterns, community agencies, systems of mental health care and delivery
2.1.2. Psychiatrists will have a working knowledge of the following:
2.1.2.1. Etiology, symptoms, course of illness, and treatment of:
2.1.2.1.1. Disruptive, impulse-control, and conduct disorders
2.1.2.1.2. Dissociative disorders
2.1.2.1.3. Elimination disorders
2.1.2.1.4. Feeding and eating disorders
2.1.2.1.5. Gender dysphoria
2.1.2.1.6. Medication-induced movement disorders
2.1.2.1.7. Neurodevelopmental disorders
2.1.2.1.8. Paraphilic disorders
2.1.2.1.9. Sexual dysfunctions
2.1.2.1.10. Sleep-wake disorders
2.1.2.1.11. Somatic symptom and related disorders
2.1.2.2. Forensics
2.1.2.3. Genetics
2.1.2.4. Medical statistics
2.1.2.5. Neuroanatomy
2.1.2.6. Neurochemistry
2.1.2.7. Pharmacology
2.1.2.8. Physiology
2.1.2.9. Public health principles
2.1.2.10. Research methodology
2.1.3. Psychiatrists will have an introductory knowledge of the following:
2.1.3.1. Complementary and alternative care modalities
2.2. Describe the CanMEDS framework of competencies relevant to Psychiatry
2.3. Demonstrate proficiency in applying lifelong learning skills of the Scholar Role to implement a personal program to keep up-to-date and enhance areas of professional competence
2.4. Demonstrate proficiency in integrating the available best evidence and best practices to enhance the quality of care and patient safety in psychiatric practice
3. Perform a complete and appropriate assessment of a patient
3.1. Establish and maintain an effective working relationship
3.2. Identify and explore issues to be addressed in a patient encounter effectively, including the patient’s context, preferences, and relevant safety issues
3.3. Perform an appropriate and accurate mental status examination for the purposes of diagnosis, management, health promotion, and disease prevention
3.4. Perform an appropriate and accurate diagnostic family interview for the purposes of diagnosis, management, health promotion, and disease prevention
3.5. Perform a focused physical or neurological examination that is relevant and accurate for the purposes of diagnosis, management, health promotion, and disease prevention
3.6. Demonstrate proficiency in selecting appropriate investigative methods in a resource-effective and ethical manner, including:
3.6.1. Medical investigation or consultation
3.6.2. Collateral information gathering
3.7. Demonstrate working knowledge of the selection of appropriate investigative methods in a resource effective and ethical manner, including but not limited to:
3.7.1. Psychological investigations
3.7.2. Questionnaires
3.7.3. Neuropsychological investigations
3.7.4. Neuroimaging
3.8. Demonstrate proficiency in effective clinical problem solving and judgment to address patient problems, including interpreting available data and integrating information to generate differential diagnosis and management plans
3.8.1. Integrate and present a biopsychosocial understanding
3.8.2. Develop and implement an integrated biopsychosocial treatment plan
4. Use preventive and therapeutic interventions effectively
4.1. Demonstrate proficiency in implementing effective management plans in collaboration with patients and their families, including:
4.1.1. Developing and implementing an integrated biopsychosocial treatment plan
4.1.2. Assessing suitability for and prescribing appropriate psychopharmacological treatments across the lifespan
4.1.3. Assessing suitability for and prescribing and delivering appropriate somatic treatments across the lifespan, including but not limited to electroconvulsive therapy (ECT)
4.1.4. Demonstrate proficiency in assessing suitability for and prescribing and delivering appropriate psychological treatments, including:
4.1.4.1. Cognitive behavioural therapy, and working knowledge of the other
4.1.4.2. Family or group therapy
4.1.4.3. Psychodynamic therapy
4.1.4.4. Supportive therapy
4.1.5. Demonstrate working knowledge in assessing suitability for and prescribing and delivering appropriate psychological treatments, including:
4.1.5.1. Behavioural therapy
4.1.5.2. Dialectic behaviour therapy
4.1.5.3. Family or group therapy, and proficiency in the other
4.1.5.4. Interpersonal therapies
4.1.6. Demonstrate introductory knowledge in assessing suitability for, prescribing, and delivering appropriate psychological treatments, including but not limited to:
4.1.6.1. Brief psychodynamic psychotherapy
4.1.6.2. Mindfulness training
4.1.6.3. Motivational interviewing
4.1.6.4. Relaxation
4.1.7. Demonstrate a proficiency in assessing and managing treatment of emergent side effects across the lifespan in each of psychopharmacological, somatic, and psychological therapies
4.1.8. Demonstrate proficiency in assessing and managing treatment adherence
4.2. Demonstrate effective, appropriate, and timely application of preventative interventions relevant to Psychiatry, including consideration of risk and safety
4.3. Demonstrate effective, appropriate, and timely application of therapeutic interventions relevant to Psychiatry, including consideration of risk and safety
4.4. Ensure appropriate informed consent is obtained for therapies
4.5. Ensure patients receive appropriate end-of-life care
5. Demonstrate proficient and appropriate use of procedural skills, both diagnostic and therapeutic
5.1. Demonstrate effective, appropriate, and timely performance of diagnostic procedures relevant to Psychiatry, including but not limited to diagnostic interviewing, questionnaire administration, and neuroimaging interpretation
5.2. Demonstrate effective, appropriate, and timely performance of therapeutic procedures relevant to Psychiatry, including but not limited to:
5.2.1. Crisis intervention, de-escalation, or nonviolent intervention techniques
5.2.2. Electroconvulsive therapy (ECT)
5.3. Ensure appropriate informed consent is obtained for procedures
5.4. Document and disseminate information related to procedures performed and their outcomes
5.5. Ensure adequate followup is arranged for procedures performed
6. Seek appropriate consultation from other health professionals, recognizing the limits of their expertise
6.1. Demonstrate insight into their own limits of expertise
6.2. Demonstrate effective, appropriate, and timely consultation of another health professional as needed for optimal patient care
6.3. Arrange appropriate followup care services for patients and their families/caregivers
Communicator
Definition:
As Communicators, Psychiatrists effectively facilitate the doctor-patient relationship and the dynamic exchanges that occur before, during, and after the medical encounter. Psychiatrists enable patient-centred therapeutic communication through shared decisionmaking and effective, dynamic interactions with patients, families, caregivers, other professionals, and others. The competencies for this role are essential for establishing rapport and trust, formulating a diagnosis, delivering information, striving for mutual understanding, and facilitating a shared plan of care. This is a central skill relevant to the practice of Psychiatry across the lifespan.
Key and Enabling Competencies: Psychiatrists are able to…
- Develop rapport, trust, and ethical therapeutic relationships with patients and families
1.1. Recognize that being a good communicator is a core clinical skill for Psychiatrists, and that effective physician-patient communication can foster patient satisfaction, adherence, and improved clinical outcomes, in addition to physician satisfaction
1.1.1. Use expert oral and non-verbal communication
1.1.2. Convey an attitude that is non-judgmental
1.2. Establish positive therapeutic relationships with patients and their families that are characterized by understanding, trust, respect, honesty, and empathy
1.3. Respect patient confidentiality, privacy, and autonomy
1.4. Listen effectively
1.5. Be aware of and responsive to nonverbal cues
1.6. Facilitate a structured clinical encounter effectively
2. Elicit and synthesize relevant information accurately, as well as the perspectives of patients and families, colleagues, and other professionals
2.1. Gather information about a disease and about a patient’s beliefs, concerns, expectations, and illness experience
2.2. Seek out and synthesize information from other sources, such as a patient’s family, caregivers, and other professionals
3. Convey relevant information and explanations accurately to patients and families, colleagues, and other professionals
3.1. Deliver information to a patient and family, colleagues, and other professionals in a humane manner and in such a way that it is understandable and encourages discussion and participation in decision-making
4. Develop a common understanding on issues, problems, and plans with patients, families, and other professionals to develop a shared plan of care
4.1. Identify and effectively explore problems to be addressed from a patient encounter, including the patient’s context, responses, concerns, and preferences
4.2. Respect diversity and difference, including but not limited to the impact of gender, religion, and cultural beliefs on decision-making
4.3. Encourage discussion, questions, and interaction in the encounter
4.4. Engage patients, families, and relevant health professionals in shared decisionmaking to develop a plan of care
4.5. Address challenging communication issues effectively, including but not limited to obtaining informed consent, delivering bad news, disclosing adverse medical events, and addressing anger, confusion, and misunderstanding
5. Convey oral and written information effectively about a psychiatric encounter
5.1. Maintain clear, concise, accurate, appropriate, and timely records of clinical encounters and plans
5.2. Present oral reports of clinical encounters and plans
5.3. Convey medical information appropriately to ensure safe transfer of care
5.4. Present medical information effectively to the public or media about a medical issue
Collaborator
Definition:
As Collaborators, Psychiatrists work effectively within a health care team to achieve optimal patient care. Psychiatrists work in partnership with others who are appropriately involved in the care of individuals or specific groups of patients. This is increasingly important in a modern multi-professional environment, where the goal of patient-centred care is widely shared. It is therefore essential that Psychiatrists are able to collaborate effectively with patients and a multidisciplinary or interdisciplinary team of expert health professionals for the provision of optimal patient care, education, and scholarship.
Key and Enabling Competencies: Psychiatrists are able to…
- Participate effectively and appropriately in an interprofessional health care team
1.1. Describe the Psychiatrist’s roles and responsibilities to other professionals within the health care team
1.2. Describe the roles and responsibilities of other professionals within the health care team
1.3. Recognize and respect the diversity of roles, responsibilities, and competencies of other professionals in relation to their own
1.4. Work with others to assess, plan, provide, and integrate care for individuals and groups of patients
1.4.1. Demonstrate the ability to provide treatment collaboratively with physicians providing primary care and understand the roles and contributions of these physicians
1.4.2. Describe the roles and contributions of workplaces, schools, forensic services, complex care facilities, and other agencies as part of a continuum of service
1.5. Work with and learn from others to assess, plan, and review other tasks, such as research problems, educational work, program review, or administrative responsibilities
1.6. Participate in interprofessional team meetings
1.7. Enter into interdependent relationships with other professionals for the provision of quality care
1.8. Identify, recognize, and describe principles of group/system dynamics
1.9. Respect team ethics, including confidentiality, resource allocation, and professionalism
1.10. Demonstrate leadership in the health care team, as appropriate
2. Work with other health professionals effectively to prevent, negotiate, and resolve interprofessional conflict
2.1. Demonstrate a respectful attitude towards other colleagues and members of an interprofessional team
2.2. Work with other professionals to prevent conflict
2.3. Employ collaborative negotiation to resolve conflicts
2.4. Respect differences and address misunderstandings and limits of scope of practice in other professions
2.5. Recognize one’s own differences, misunderstandings, and limitations that may contribute to interprofessional tension
2.6. Reflect on interprofessional team function
Leader
Definition:
As Leaders, Psychiatrists are integral participants in health care organizations, organizing sustainable practices, making decisions concerning the allocation of resources, and contributing to the effectiveness of the health care system.
Key and Enabling Competencies: Psychiatrists are able to…
- Participate in activities that contribute to the effectiveness of their health care organizations and systems
1.1. Work collaboratively with others in their organizations
1.2. Participate in systemic quality process evaluation and improvement, including patient safety initiatives
1.3. Describe the structure and function of the health care system as it relates to Psychiatry, including the roles of physicians
1.4. Describe principles of health care financing, including physician remuneration, budgeting, and organizational funding
2. Manage their practice and career effectively
2.1. Set priorities and manage time to balance patient care, practice requirements, outside activities, and personal life
2.2. Manage a practice, including finances and human resources
2.3. Implement processes to ensure personal practice improvement
2.4. Employ information technology appropriately for patient care
3. Allocate finite health care resources appropriately
3.1. Recognize the importance of just allocation of health care resources, balancing effectiveness, efficiency, and access with optimal patient care
3.2. Apply evidence and management processes for cost-appropriate care
4. Serve in administration and leadership roles, as appropriate
4.1. Chair or participate effectively in committees and meetings
4.2. Lead or implement change in health care
4.3. Plan relevant elements of health care delivery, such as work schedules
Health Advocate
Definition:
As Health Advocates, Psychiatrists use their expertise and influence responsibly to advance the health and well-being of individual patients, communities, and populations.
Key and Enabling Competencies: Psychiatrists are able to…
- Respond to individual patient health needs and issues as part of patient care
1.1. Identify the mental health needs of an individual patient
1.2. Identify opportunities for advocacy, health promotion, and disease prevention with individuals to whom they provide care, demonstrating knowledge of:
1.2.1. Major regional, national, and international advocacy groups in mental health care
1.2.2. Governance structures in mental health care
1.2.3. Legal issues in mental health care
2. Respond to the health needs of the communities that they serve
2.1. Describe the practice communities that they serve
2.2. Identify opportunities for mental health advocacy, health promotion, and disease prevention in the communities that they serve, and respond appropriately
2.3. Demonstrate an appreciation of the possibility of competing interests between the communities served and other populations
3. Identify the determinants of mental health for the populations that they serve
3.1. Identify the determinants of mental health of the population, including barriers to access to care and resources
3.2. Identify vulnerable or marginalized populations within those served and respond appropriately
4. Promote the health of individual patients, communities, and populations
4.1. Describe an approach to implementing a change in a determinant of health of the populations they serve
4.2. Describe how public policy impacts on the health of the populations served
4.3. Identify points of influence in the health care system and its structure
4.4. Describe the ethical and professional issues inherent in health advocacy, including altruism, social justice, autonomy, integrity, and idealism
4.5. Demonstrate an appreciation of the possibility of conflict inherent in their role as a health advocate for a patient or community with that of manager or gatekeeper
4.6. Describe the role of the medical profession in advocating collectively for health and patient safety
Scholar
Definition:
As Scholars, Psychiatrists demonstrate a lifelong commitment to reflective learning, as well as the creation, dissemination, application, and translation of medical knowledge.
Key and Enabling Competencies: Psychiatrists are able to…
- Maintain and enhance professional activities through ongoing learning
1.1. Describe the principles of maintenance of competence
1.2. Describe the principles and strategies for implementing a personal knowledge management system
1.3. Recognize and reflect on learning issues in practice
1.4. Conduct a personal practice audit
1.5. Pose an appropriate learning question
1.6. Access and interpret the relevant evidence
1.7. Integrate new learning into practice
1.8. Evaluate the impact of any change in practice
1.9. Document the learning process
2. Critically evaluate medical information and its sources, and apply this appropriately to practice decisions
2.1. Describe the principles of critical appraisal
2.2. Critically appraise retrieved evidence in order to address a clinical question
2.3. Integrate critical appraisal conclusions into clinical care
3. Facilitate the learning of patients, families, students, residents, other health professionals, the public, and others
3.1. Describe principles of learning relevant to medical education
3.2. Identify collaboratively the learning needs and desired learning outcomes of others
3.3. Select effective teaching strategies and content to facilitate others’ learning
3.4. Deliver effective lectures or presentations
3.5. Assess and reflect on a teaching encounters
3.6. Provide effective feedback
3.7. Describe the principles of ethics with respect to teaching
4. Contribute to the development, dissemination, and translation of new knowledge and practices
4.1. Describe the principles of research and scholarly inquiry
4.2. Describe the principles of research ethics
4.3. Pose a scholarly question
4.4. Conduct a systematic search for evidence
4.5. Select and apply appropriate methods to address the question
4.6. Disseminate the findings of a study
4.7. Participate in a scholarly research, quality assurance, or educational project relevant to Psychiatry, demonstrating primary responsibility for at least one of the following elements of the project:
– Development of the hypothesis, which must include a comprehensive literature review
– Development of the protocol for the scholarly project
– Preparation of a grant application
– Development of the research ethics proposal
– Interpretation and synthesis of the results
Professional
Definition:
As Professionals, Psychiatrists are committed to the health and well-being of individuals and society through ethical practice, profession-led regulation, and high personal standards of behaviour.
Key and Enabling Competencies: Psychiatrists are able to…
- Demonstrate a commitment to their patients, profession, and society through ethical practice
1.1. Exhibit appropriate professional behaviours in practice, including honesty, integrity, commitment, compassion, respect, and altruism
1.2. Demonstrate a commitment to delivering the highest quality care and maintenance of competence
1.3. Recognize and appropriately respond to ethical issues encountered in Psychiatry
1.4. Recognize and manage real or perceived conflicts of interest, including but not limited to interaction with industry
1.5. Recognize the principles and limits of patient confidentiality as defined by professional practice standards and the law
1.6. Maintain appropriate relationships with patients, colleagues, and students, and demonstrate professionalism that adheres to the principles respecting boundaries in all areas of interaction, specifically including sexual and financial matters
2. Demonstrate a commitment to their patients, profession, and society through participation in profession-led regulation
2.1. Demonstrate knowledge and understanding of the professional, legal, and ethical codes of practice
2.1.1. Abide by accepted guidelines, including but not limited to those that pertain to ethical interactions with industry, especially the pharmaceutical industry, with respect to research, education, and clinical care
2.2. Fulfil the regulatory and legal obligations required of current practice
2.3. Demonstrate accountability to professional regulatory bodies
2.4. Recognize and respond to others’ unprofessional behaviours in practice
2.5. Participate in peer review
3. Demonstrate a commitment to physician health and sustainable practice
3.1. Balance personal and professional priorities to ensure personal health and a sustainable practice
3.2. Strive to heighten personal and professional awareness and insight
3.3. Recognize other professionals in need and respond appropriately

